Mucus is a thin, sticky substance that lines many parts of your body including the mouth, sinuses, and lungs. In the lungs, mucus plays a key role in protecting your lungs and airways from harmful irritants.
Key Facts:
- Sputum and phlegm are other names sometimes used to refer to the mucus in your lungs and airways.
- Changes in mucus amount, thickness or color may be a sign of infection or another health condition.
- A sputum culture is a test that checks for bacteria or other types of germs that may be causing an increase in mucus.
Why Do We have Mucus?
In healthy lungs, your airways are lined with a thin layer of mucus and tiny hairs called cilia. The mucus and cilia trap irritants, like germs, dust, or smoke, before it can get into your lungs. When you cough, it helps remove these irritants from your body. This also protects you from germs that may cause an infectious lung disease like the flu or COVID-19.
If you are living with a chronic lung disease like COPD, cystic fibrosis, or bronchiectasis it may mean you have more, thicker or stickier mucus in your lungs. When mucus collects in your airways it can make breathing harder and increase your risk of getting an infection.
When Should I Seek Medical Attention?
If an increase in mucus production is a new or worsening symptom for you, you may be experiencing a lung infection. Some additional signs or symptoms include fever, cough that produces mucus, shortness of breath, or chest pain.
If your healthcare provider suspects you have a respiratory infection, they may order a sputum culture* to analyze a sample of your sputum or phlegm for bacteria or fungi. A sputum culture can also help diagnose respiratory conditions like pneumococcal pneumonia or bronchiectasis. Depending on your symptoms, they may also order a chest X-ray or CT scan.
*To perform a sputum culture, you will be asked to cough up mucus into a cup or container. The mucus will be analyzed in a lab, and you may get your results in a few days or a few weeks. If you are having trouble coughing up enough mucus, your provider may ask you to breathe in a saline solution or mist. This mist may help you cough up the mucus more easily. If you are still having trouble bringing up enough mucus, your provider may order a bronchoscopy.
The colors of your mucus can give a picture of what is happening in your lungs. Normal mucus color may appear clear, white or gray. If your mucus is white with a yellow tint, yellow or green, this may be a sign of an infection. Your mucus may also be pink, red, dark brown or black. These colors may be a more serious health condition or sign of infection. You should see your healthcare provider right away if you have changes in the color of your mucus or have other symptoms.
Treating and Managing Mucus
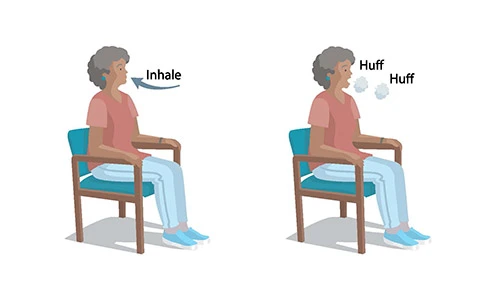
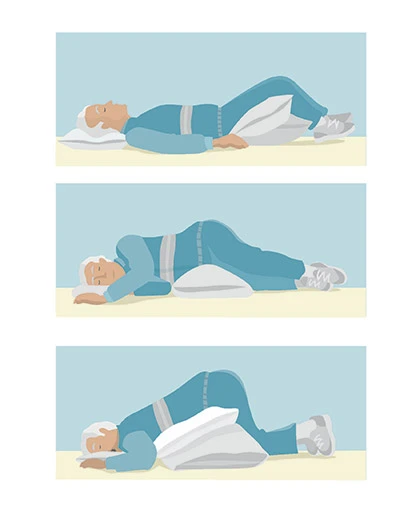
If you have excess mucus production or this is a new symptom, there are steps you can take to help prevent and remove the mucus in your lungs. You and your healthcare provider should work together to find a strategy and monitor the progress. Your healthcare provider may recommend you try to:
Living with a chronic lung disease can be challenging. The American Lung Association has support programs available to help you.
- Attend a Better Breathers Club meeting to get support from others living with lung disease.
- Join the Patient & Caregiver Network and access to information that may help you better manage your lung disease and improve your lung health.
- Find an online support community through Inspire and get support from other people living with chronic lung disease.
- Contact the HelpLine (800-LUNG-USA) and have your lung disease questions answered by medical professionals like respiratory therapists or nurses.
- Receive free, personalized, one on one asthma and COPD education and support through the Lung Health Navigator.
Resources
Page last updated: January 15, 2026